Coming soon to a clinic near you
Data, AI & machine learning
AI is being used in diagnostics, patient monitoring, the development of personalized treatment plans and more. Machine learning models will predict the likelihood of diseases based on patient data, leading to earlier and more accurate diagnoses. For most physicians, the true power will come when AI scribes are fully integrated with EMRs.
“These bots will be able to scour through 20,000 studies in a matter of seconds and summarize things for you at the point of care,” said Muhammad Mamdani, vice-president of data science and advanced analytics at Unity Health Toronto. “There are programs that look through the Canadian guidelines that nobody can seem to remember, for example, and say, ‘well, according to Canadian guidelines on managing depression, for patients who went through this antidepressant and had failure, the next step is to try X.’”
CHARTWatch, in partnership with Canadian health AI startup
Signal 1, is an example of AI and machine learning being used in several hospitals. It takes huge amounts of data sets, such as diagnostic test results and patient vitals over time and analyzes when people have decompensated. It’s used to predict the level of support a patient will need and when a patient is going to decompensate and sends a warning to nurses and doctors. Preliminary data show that ChartWatch, now also used in surgical units, has decreased mortality by 20% in Toronto’s St. Michael’s Hospital general internal medicine unit.
Personalized medicine
AI can recommend personalized treatment plans by analyzing guidelines, a patient’s medical history, genetic data and current condition and environment. By analyzing vast datasets of morphological data, AI algorithms can uncover hidden patterns and connections, identifying previously unknown disease markers and pave the way for earlier, more precise diagnoses.
“It will tell you for a 60-year-old female with X, Y and Z conditions, this is the recommended treatment option, which is different than if you were a 72-year-old male,” said Mamdani. “It is looking at success patterns of other patients. It would be able to scour all the data to say, ‘Most of the time when you tried X, it worked. When you tried Y, it didn’t, so I would favour X for this patient.’”
Dr. Andrew Pinto is a family physician in Toronto and founder and director of the Upstream Lab, which is researching using data science to enable learning health systems. “We follow provincial guidelines around breast cancer and colon cancer screening. We know that people have very different risk levels based on family history, genetics, social circumstances and existing health conditions. But we don’t have a simple way to put that together, and this is where AI tools could be very helpful—integrating all of these pieces into a tailored prescription for that individual.”
Education & training
It can be challenging for busy physicians to keep up with current advances, evolving technologies and treatments. Since AI can work with huge volumes of information, it can scan medical journals and guidelines to highlight the most relevant to an individual practitioner. Not only that, it will even be able to suggest courses best suited to individual physicians.
“What we’ll see in the next five or 10 years, is much more integration of tools that drive continuing medical education,” said Dr. Pinto. “(Your EMR) could say, ‘if we look at your practice, this course would benefit you and here are the upcoming opportunities in your city,’” he said, giving the example of a physician who has many patients with early onset dementia, and the EMR announcing an upcoming course at the local university. “The system could work in the other direction, too, where this type of data could inform what sessions should be given at universities and conferences.”
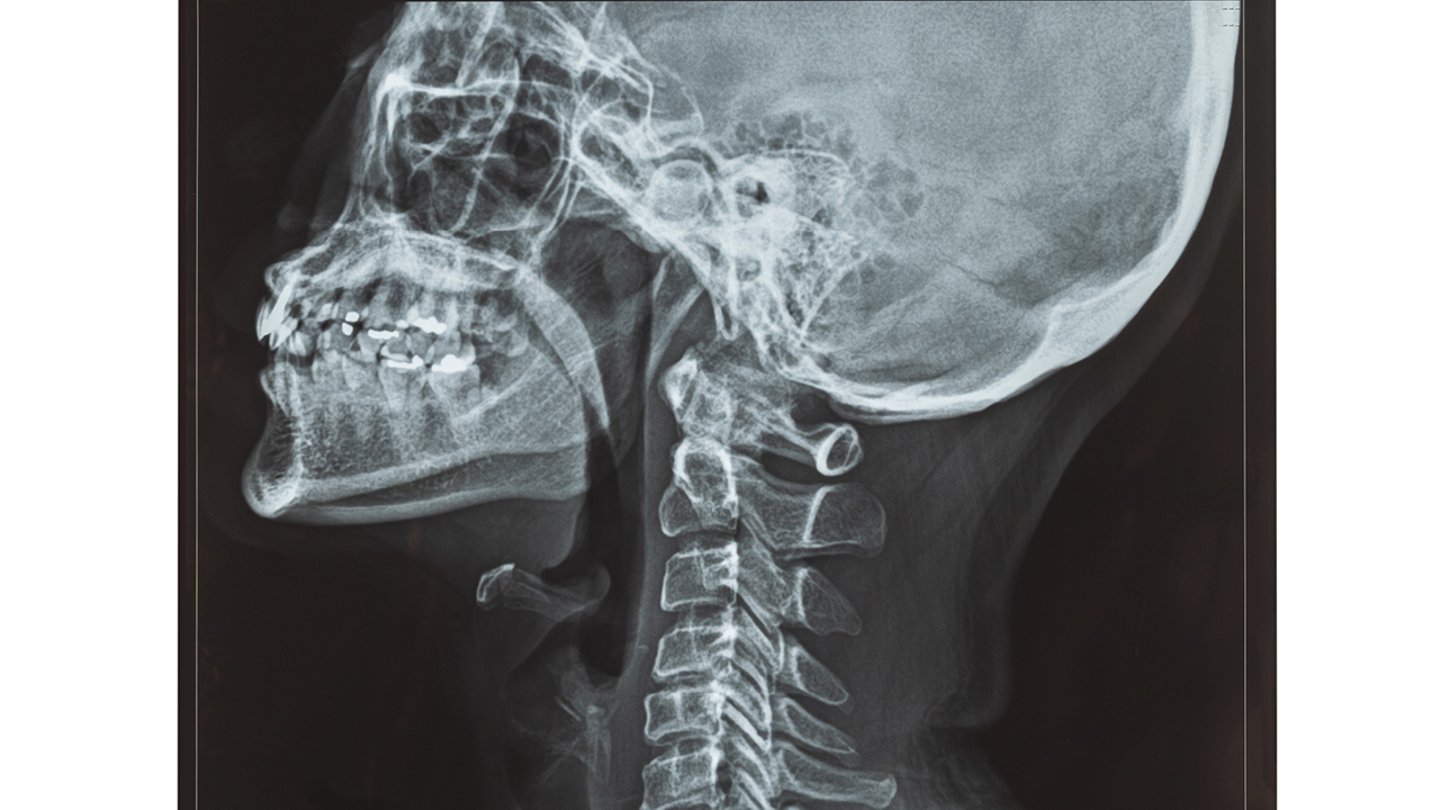
Medical imaging
The science says that AI algorithms can analyze X-rays, MRIs and CT scans more quickly and accurately than human radiologists, detecting abnormalities such as tumours, fractures and infections. This isn’t to say radiologists are not needed to look at the images, but that AI can flag the urgent cases that need immediate attention.
Dr. Alun Ackery is an emergency physician at St. Michael’s Hospital and is involved in AI to improve efficiencies and outcomes. Dr. Ackery explained that in less than two minutes of a head CT being done, AI will alert the team whether there’s a bleed or not, before the radiologist has looked at it. The next step (not yet in use) is to have AI then determine if the bleed needs surgery, warranting a call to the neurosurgeon.
“If someone has a head bleed in Barrie, (Ont.,) they don’t have a neurosurgeon there, so they have to call a hospital like St. Mike’s. Neurosurgeons get about 18,000 calls a year, far more than any other specialists. Currently, ED physicians are having to connect with these specialists when sometimes it’s very unlikely the patient’s going to need surgery,” Dr. Ackery said.
The tool will save time for ED physicians and neurosurgeons and get patients more quickly to where they need to be. “This is of massive clinical importance for emergency physicians because . . . it saves time. It’s going to help our system be more efficient.” The Unity Health team is also looking at similar tools for kidney stones, spine injuries and other trauma patients.
Voice diagnosis
Another exciting technology for healthcare involves voice diagnostics. A collaboration between Pfizer and IBM, for example, is using sensors and mobile devices to measure Parkinson’s symptoms, by analyzing speech patterns, variance in pitch, word choice, grammar, vocal cord tremors, breathiness and weakness. A recent research collaboration between the Mayo Clinic and Beyond Verbal, an Israeli voice-analytics company, suggests the voice may also hold clues to detecting coronary artery disease. Scientists at Toronto’s Klick Labs are testing an AI-powered program they developed to immediately detect type 2 diabetes using less than 10 seconds of voice recording.
Meanwhile, a collaboration of 10 North American universities, including the University of Montreal, Simon Fraser University in Burnaby, B.C., and SickKids in Toronto, is studying “Voice as a Biomarker of Health,” a project to build an ethically sourced database of diverse human voices. Using this data, machine learning models will be trained to spot diseases by detecting changes in the human voice, for neurological, mood, psychiatric and respiratory disorders and pediatric voice and speech disorders.
Robotic surgery
AI is also revolutionizing the field of surgery, so much so that accounts of robotic surgery “firsts” are regularly in the news, such as the recently reported first Canadian robot-assisted direct lateral spine surgery at London Health Sciences Centre in London, Ont. AI-powered robots can be programmed to perform complex procedures with greater precision and accuracy than surgeons. There is potential for this to lead to cost savings, shorter wait times and shorter surgery times, with less pain and scarring and improved outcomes. Robotics are now regularly used for hip and knee replacements, thoracic surgery, neurosurgery and urologic and gynecologic procedures.
Meanwhile, Dr. Amin Madani, a general surgeon at the University Health Network in Toronto, has developed a prototype that uses AI to guide surgeons during gallbladder surgery. The prototype uses computer vision—AI that trains computers to interpret images—to identify in real-time areas of an organ that are safe to dissect and those that are not.
Patient self-care
As patients aim to take more control of their health, there is no shortage of apps, bots and wearables (in the form of watches, rings and bracelets) available or soon-to-be-available to help. AI-powered chatbots can provide patients with information, answer questions and offer support, improving patient engagement and satisfaction. AI applications, such as Wobot, can provide mental health support through chatbots and apps that offer counseling, monitor mood, suggest coping strategies and alert the patient when they should see a doctor.
Mamdani said that these tools will be able to respond when a patient says, for example, “Robot (or phone app), I have my lab results and access to my medical records. Why don’t you look at those? I’m also going to link you up to my Apple Watch.’ We’re going to see more and more sensors with biometrics and AI can say, ‘Last night when you were sleeping, I noticed a bit of a skip in your heart rate. You may want to get that checked out.’”
Hospital at-home
Virtual wards or hospitals at home are expected to continue to grow across the country and are credited with reducing patient stress (and helping recovery) while easing hospital crowding and costs. Quebec recently announced it is expanding its Hospital at Home program, pioneered at Montreal’s Jewish General Hospital during the pandemic, to five more hospitals, and B.C. hospitals like Vancouver General Hospital already have robust hospital-at-home programs that rely on AI and wearable sensors that monitor vital signs in real-time, alerting patients and doctors to potential health issues before they become critical.
“If you put the right sensors on a patient, you can monitor them remotely and AI will keep track of them every second of the day, literally,” said Mamdani, “rather than a human who can only be there half the time.”